
The Barrier Function of the Gut
Let's delve into the intriguing world of the gut mucosa and its tight junctions! Picture the gut mucosa as a protective lining of cells that covers and safeguards our intestines from the external environment. It serves as a diligent security team, ensuring that undesirable elements are kept at bay while allowing beneficial substances to pass through.
Within this lining, there exists a space known as the gut lumen, where various molecules are secreted and immune cells come into play. Their combined efforts fortify the barrier function of the gut mucosa, defending against harmful microbes, toxins, and other unwanted intruders. It's akin to having a formidable army of defenders on constant alert, prepared to eliminate any potential threats.
Now, let's turn our attention to the remarkable tight junctions, often referred to as TJs. These structures are the stars of the show within the intestinal wall, playing a vital role not only during normal, healthy conditions but also in response to pathological situations.
Believe it or not, there are more than 150 proteins involved in the intricate workings of these tight junctions. Their collective efforts are akin to a well-coordinated symphony, with each protein fulfilling its designated role to maintain the integrity and functionality of the intestinal barrier. Now, here comes the fascinating part. Among these proteins, there is one significant player called zonulin, which acts as the conductor of the tight junction orchestra. Zonulin possesses the remarkable ability to regulate the permeability of the gut, determining how easily substances can pass through the intestinal barrier.
Imagine Zonulin as a pivotal character who occasionally stirs things up. It's as though it opens the doors of the intestinal barrier a bit wider, allowing a greater influx of substances than usual. While this phenomenon isn't always detrimental, it can introduce a certain level of disruption within the gut.
And there you have it—a glimpse into the world of the gut mucosa, tight junctions, and the influential zonulin protein. It showcases the delicate equilibrium between fortifying our defenses and selectively allowing beneficial elements to pass through. Our bodies possess an array of intricate mechanisms, and participants collaborate harmoniously to uphold our well-being and ensure proper functionality.

Gut Microbiome
The microbiome indicates the collection of all microorganisms, including bacteria, fungi, viruses, and their genes, that exist naturally on and within our bodies. Our small and large intestines contain the majority of the body's microorganisms.
The gut microbiota is vital for digestion as well as immune system function. Disruptions in the gut microbiota can lead to illness.
The gut microbiota contains more bacteria than the total number of cells in the human body.
What is Gut Dysbiosis?
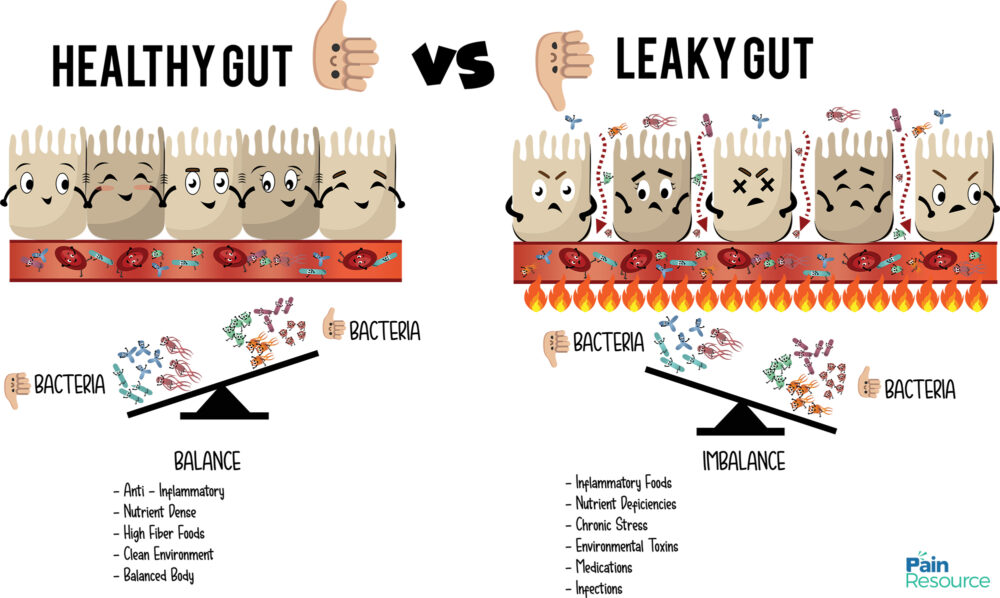
"Dysbiosis" is a term used to indicate a lack of adaptation or imbalance inside the body, and "gut dysbiosis" happens when there is an imbalance in the amount and variety of your gut microbiota (overgrowth of bad bacteria and less good bacteria).
Gut dysbiosis produces increased zonulin with a significant loss in gut barrier function. It causes the release of inflammatory agents into the intestine, resulting in increased permeability for dietary and microbial agents.

Potential Triggers
Unbalanced Diet
- Excess of sugar, protein, fat
- Industrial foods
- Insufficient plant foods
- Usage of hydrogenated fats
- Omega3 & omega6 fatty acids ratio imbalance

Bad Eating Habits
- Improper chewing
- Excessive alcohol drinking
- Frequent food outlets
Medications
- Antibiotics
- Antacids
- Contraceptive pills
Consequences of Dysbiosis
They are numerous and not limited to the digestive tract. They can induce ENT problems, skin problems, allergies, weight gain or obesity, and depression.
How does the Gut get Leaky?
- The immune response arises from the interplay of genes and the environment. The gut has most of the immune cells.
- When the gut microbiome becomes unbalanced, with more bad bacteria than good bacteria, our immune system gets activated. Bacteria and toxins in the intestines may sometimes pass through the walls and reach the bloodstream.
- A leaky gut is due to a decline in the barrier function of the gut mucosa, which leads to huge holes in the lining.
- As a result, restricted materials (for example, proteins, gluten, bacteria, and food antigens) can now flow through tissue and the bloodstream.
Leaky Gut Symptoms
- Bloating, discomfort, and other digestive issues.
- Pain in the abdomen
- Many people have dietary intolerance, sensitivities, or allergies.
Consequences of Leaky Gut
Chronic inflammation results in an imbalance of the following systems:
- Endocrine system: Disturbed hormonal secretions.
- Immune system: Our immune cells are responsible for recognizing ourselves and eliminating anything that is foreign bodies. Our microbiota is our body's first line of defense. We are more prone to become infected since it loses the ability to defend our bodies.
- Nervous system: Our intestines contain more neurons than our brains! Toxins produced by opportunistic bacteria (often dangerous) paralyze the muscular nerve cells in our intestines and cause pain, abdominal distension, and difficulty in passing stools. Furthermore, when these opportunistic bacteria encounter one another, they create a shell where minerals and metals accumulate.
Combined Effects of Dysbiosis and Leaky Gut
Passage of harmful bacteria and inflammation-causing chemicals links to the development of many chronic illnesses, including obesity, diabetes mellitus, cardiovascular, gastrointestinal, and neurological disorders, and cancers.
How can the Functional Medicine Approach help Restore Gut Health?
Although this is an oversimplification, testing for nutritional deficiencies, dysbiosis, food allergies, infections, and toxins is generally the first step in treatment. Consult with a functional medicine professional before following the list below.
- Avoid all dairy products, eggs, allergies, and wheat for two to four weeks.
- Probiotics (ingestible beneficial bacteria) reintroduce healthy bacteria.
- Deficient nutrients are restored by eating optimal meals and taking supplements.
- Slowly include other foods and closely watch if any symptoms reappear.
- Stress management, diet change, exercise, and detoxification also help.

Frequently Asked Questions (FAQs)
1. What are the symptoms of gut dysbiosis?
Common symptoms of gut dysbiosis include bloating, digestive issues, abdominal pain, food intolerances, allergies, and skin problems. Other symptoms may include weight gain or obesity, ENT problems, and mood disorders like depression.
2. How does gut dysbiosis affect the gut barrier?
Gut dysbiosis disrupts the balance of good and bad bacteria in the gut, leading to increased zonulin production and a loss of gut barrier function. This can result in increased permeability, allowing inflammatory agents and other substances to pass into the bloodstream.
3. What can cause gut dysbiosis?
Factors that can contribute to gut dysbiosis include an unbalanced diet with excess sugar, protein, or fat, consumption of industrial foods, insufficient intake of plant foods, use of hydrogenated fats, and an imbalance in omega-3 and omega-6 fatty acids. Other triggers include bad eating habits, medications like antibiotics and antacids, constipation, and unregulated stress.
4. What are the consequences of a leaky gut?
A leaky gut, caused by compromised gut barrier function, can lead to chronic inflammation, disturbances in hormonal secretions, compromised immune function, and effects on the nervous system. It is associated with various chronic illnesses such as obesity, diabetes, cardiovascular diseases, gastrointestinal disorders, neurological disorders, and certain cancers.
5. How can functional medicine help restore gut health?
Functional medicine takes a comprehensive approach to address gut dysbiosis and leaky gut. It involves testing for nutritional deficiencies, dysbiosis, allergies, infections, and toxins. Treatment may include avoiding trigger foods, introducing probiotics, restoring nutrients through diet and supplements, gradually reintroducing foods while monitoring symptoms, managing stress, making dietary changes, exercising, and supporting detoxification. Consulting with a functional medicine professional is recommended for personalized guidance.


.png)


