
Type 1 diabetes (T1D) is an organ-specific autoimmune disease characterized by the selective destruction of pancreatic β-cells. It is well known that T1D is frequently associated with other organ-specific autoimmune diseases, including Autoimmune Thyroid Disease (AITD), pernicious anemia, and idiopathic Addison’s disease. Read to know more.
Diabetes mellitus is increasing in prevalence worldwide. Type 1 diabetes is caused by a loss or malfunction of the insulin-producing cells, called pancreatic beta cells. Damage to beta cells results in the absence or insufficient production of insulin produced by the body. Most cases of type 1 diabetes have an autoimmune basis, and the immune system mistakenly attacks and destroys beta cells. Since insulin is necessary to sustain life, the missing insulin has to be replaced.

Type 1 diabetes (T1D) is a chronic autoimmune disease characterized by the loss of insulin-producing pancreatic β-cells. The pathogenesis of T1D is complex and multifactorial and involves a genetic susceptibility. Genetic background may affect the risk of autoimmune disease in patients with T1D. A patient can exhibit an increased risk of other autoimmune disorders such as autoimmune thyroid disease, Addison's disease, autoimmune gastritis, coeliac disease, and vitiligo. The most common coexisting organ-specific autoimmune disease in patients with T1D is autoimmune thyroid disease. Patients with anti-thyroid antibodies are more likely to develop thyroid disease than patients without anti-thyroid antibodies. It is reported that the presence of anti-thyroid antibodies at the diagnosis of T1D predicts the development of future thyroid disease.
Type 1 Diabetes (T1D)
Type 1 diabetes (T1D), also known as juvenile diabetes, is an autoimmune disease that originates when very little or no insulin is produced by the islets of Langerhans (containing beta cells) in the pancreas. Insulin is a hormone required for the cells to use glucose for energy, and it helps regulate glucose levels in the bloodstream. Due to low insulin production, high blood sugar levels rise in the body. Diabetes leads to the continuous flow of foods and fluids in and out of the body, because of which the person constantly feels thirsty and hungry, frequently urinates, and loses weight. Challenges in treating T1D are abnormal liver, lifelong medicine dependency, poor heart health, kidney damage, confusion about what to eat, and poor fitness.
The exact cause of type 1 diabetes is unknown, but it is known that genetic and environmental factors can cause diabetes. The main and underlying reason is autoimmune destruction: the body's own immune system, which normally fights harmful bacteria and viruses, mistakenly destroys the insulin-producing (islet, or islets of Langerhans) cells in the pancreas. Various patients successfully control their sugar levels through injections and medicine, but that's not the cure; they are only controlling half of the problem and neglecting the other half, which is more important to treat, and that is autoimmunity. If this is not treated, then the patient will suffer from other autoimmune diseases as well in the future.
Autoimmunity Disease
Autoimmune diseases refer to problems with the immune system, which usually fight off viruses, bacteria, and infections. The problem causes your immune cells to attack your body by mistake. These diseases can affect almost any part of the body. It releases proteins called autoantibodies that attack healthy cells. Some autoimmune diseases target only one organ; T1D damages the pancreas; other diseases, like Systemic Lupus Erythematosus (SLE), affect the whole body. There are around 70+ autoimmune diseases. The cause of autoimmune diseases is unknown; however, genetics, diet, infections, and exposure to chemicals might be involved.
Symptoms
Symptoms to diagnose an autoimmune disease are:
- Fatigue
- Achy muscles
- Swelling and redness
- Low-grade fever
- Trouble concentrating
- Numbness and tingling in the hands and feet
- Hair loss
- Skin rashes
Individual diseases can also have their own unique symptoms. For example, type 1 diabetes causes extreme thirst, weight loss, and fatigue. IBD causes belly pain, bloating, and diarrhea. With autoimmune diseases like psoriasis or RA, symptoms may come and go. A period of symptoms is called a flare-up. A period when the symptoms go away is called remission. If you have one type of autoimmune disease, then there are high chances of being diagnosed with other autoimmune diseases as well; therefore, it is necessary to treat autoimmunity.
Immune System
Type 1 diabetes is caused by an autoimmune process in the body that mistakenly destroys the insulin-producing cells, or beta cells, and occurs in genetically predisposed individuals. To understand the autoimmune attack of beta cells in type 1 diabetes, it is necessary to understand the functioning of the immune system. In humans, the immune system protects the person from outside invaders (also known as pathogens), such as bacteria or viruses, and abnormal or diseased cells, such as cancer cells. Additionally, the immune response allows some foreign material and normal cells for each individual (or “self”) to be tolerated. The balance between a destructive response and a tolerant response has to be correct; otherwise, people might get diagnosed with autoimmune medical problems.

The immune cells are called lymphocytes, a type of white blood cells. Lymphocytes include:
- T cells can attack or kill infected or defective cells, and also regulate the immune response. The T cell receptors (TCRs) on their cell surface recognize and respond to foreign or abnormal tissue. This process is called cell-mediated immunity.
- B cells that make antibodies. B cells are involved in humoral – related to the blood – immunity.
- NK (natural killer) cells that cause cell death.
The body has different T cells, B cells, and NK cells that can respond to foreign or abnormal tissue. T cells are selected by the thymus gland during the person’s development and respond to foreign or abnormal protein snippets presented by MHC. The major histocompatibility complex (MHC) is the mechanism by which the immune system can differentiate between self and non-self cells. They will ignore self-proteins. Only those T cells with a T cell receptor specific for the protein snippet will respond. B cells will respond to foreign protein snippets presented by MHC class molecules by forming antibodies. B cells make antibodies against a range of different protein combinations and shapes but normally do not make antibodies against self-proteins. The range of antibody responses is unique to each individual and develops over the person’s lifetime. NK cells respond automatically to foreign or diseased molecules by releasing toxic chemicals that destroy cells. This NK response is universal to all humans, which means everyone normally responds to the same things. In autoimmunity disease (T1D), beta cells start making antibodies against self-proteins (insulin-producing beta cells), and under T cells, the immune system is unable to differentiate between non-self (foreign) and self cells, resulting in the attack of own beta cells.
Autoimmunity and Type 1 Diabetes
Before the time of diagnosis, it is speculated that the regulatory T cells are unable to control cytotoxic T cells directed against self-proteins. T cells coordinate to attack and destroy insulin-producing cells (beta cells). At the same time, B cells are making antibodies against beta-cell proteins. When the number of beta cells is reduced by approximately 80%, the body is unable to secrete enough insulin, the blood sugar rises, and clinical diabetes is diagnosed.

The presence of antibodies directed against beta-cell antigens or molecules is a significant risk factor for the development of type 1 diabetes. The antibodies are directed against proteins associated with the beta cells, such as glutamic acid decarboxylase, tyrosine phosphatase, insulin, and heat shock proteins. There are various tests available to test for these antibodies, such as:
- Glutamic Acid Decarboxylase (GADAs)
- Islet Cell Antigen 512 (ICA512s or ICA IA-2s)
- Insulin Autoantibodies (IAAs)
- Islet Cell Antibodies (ICAs)
- Zinc Transporter 8 (ZnT8)
Another test is the Intravenous Glucose Tolerance Test (IVGTT), which evaluates “first phase” insulin secretion. “First phase” refers to the amount of insulin secreted within the first few minutes after the administration of the intravenous glucose. When someone has a low first-phase insulin secretion and two or more antibody tests are positive, there is at least a 90% risk of developing clinical diabetes within the next few years.
Genetics
Type 1 diabetes is a complex genetic disorder. It occurs more frequently in families in which there are other relatives with type 1 diabetes and other autoimmune conditions. Children have a 5% to 6% chance of developing diabetes if their father has type 1 diabetes, and a 3% to 4% chance if their mother has type 1 diabetes. If a sibling has type 1 diabetes, the risk is 5-6%; however, if the sibling has identical MHC (Major Histocompatibility Complex), the risk increases. When one identical twin has diabetes, the risk of the other twin developing diabetes has been thought to be about 40%. Several genes have been identified that are associated with the development of diabetes. The chromosomal locations of these “diabetes genes” are called inherited susceptibility loci.
Associated Autoimmune Disease
There are a few autoimmune diseases that tend to co-occur with Type 1 diabetes which are listed below.
- Celiac disease
- Thyroid disease
- Multiple sclerosis
- Lupus
- Gastritis
- Addison’s disease
- Vitiligo
- Autoimmune arthritis
Conventional Treatment
Type 1 diabetes and other chronic diseases are termed incurable in the sense that there is no permanent cure in allopathy; however, this might be true in allopathy, but it is not in other medicinal fields. Insulin injections and eating medicines are not enough to cure T1D; this only helps in keeping blood sugar levels under control and not treating the underlying cause. Some people undergo Isle Transplant surgery or other surgeries to replace defective islets with new and healthy islets; this is a short-term relief as the patient's autoimmunity is still not treated. After some years, the person will again show symptoms of T1D because the immune system will again start attacking insulin-producing beta cells. In functional medicine, autoimmunity is cured, and as a result, T1D, termed incurable, is completely cured.
Functional Medicine
Functional medicine is one of the ways to cure or reverse all kinds of ailments, including T1D. In this, doctors find the root cause of the illness and focus on the genes, the environment, the person's biological health, and their mental health; in short, the overall nature and being of the patient. This makes it easy to treat the patient appropriately and not just focus on managing or controlling the symptoms.
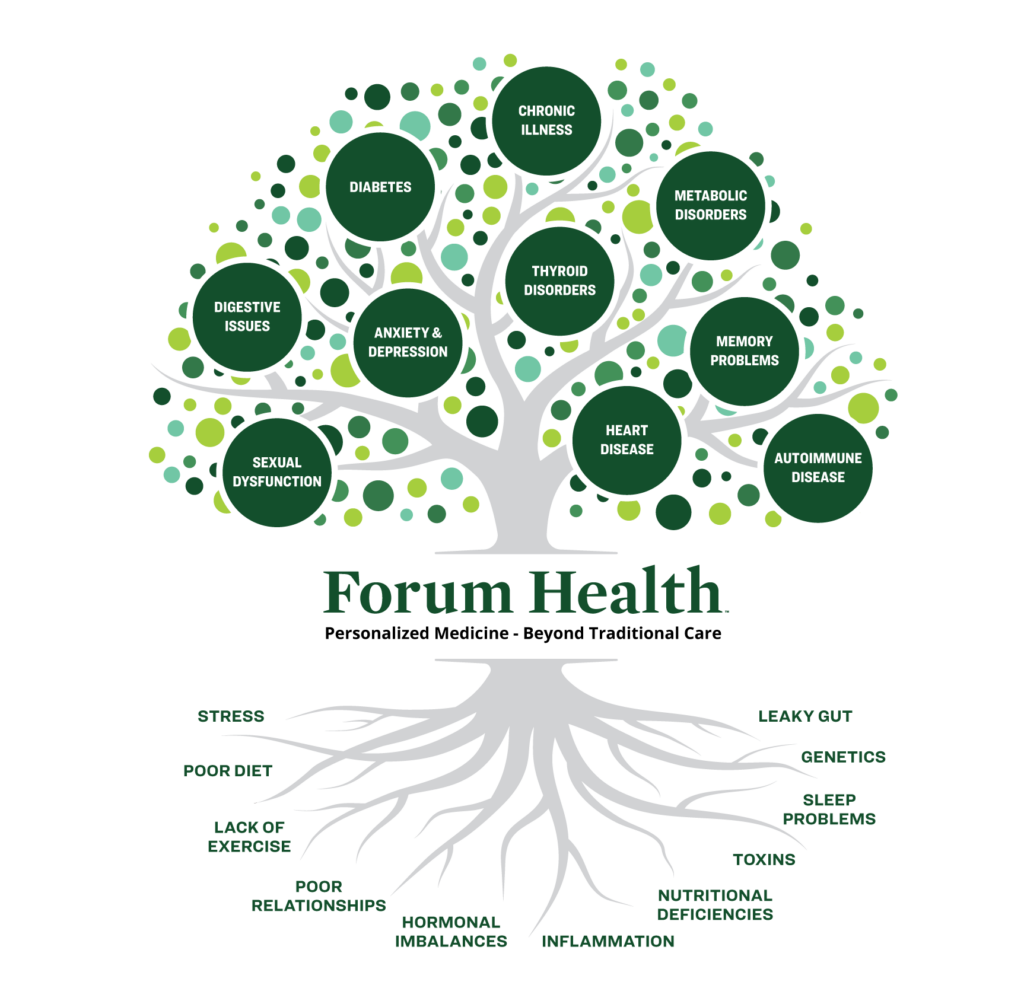
There are two things that need to be kept in mind while treating T1D: first, to maintain a sugar level between 5.8 and 6.2 in children so that their energy levels are proper, they get efficient sleep, and they don't suffer from fatigue or other complications. The second is to keep autoimmunity under control so that the patient is protected from other autoimmune conditions. If these two things are perfectly managed and controlled, then the pancreas starts to heal itself and function efficiently. There are four stages of recovery.
- Contain HbA1c to less than 6: This means to control blood sugar level, that's the first step so that it becomes easy to proceed further.
- Clean Internal Environment: Eliminate all the toxins, deficiencies, insufficiencies, leaky gut syndrome, inflammation, and oxidative stress through a proper and balanced diet.
- Address Autoimmunity: This is done by Coimbra's Protocol, where a high dose of Vitamin D is given to recover and strengthen our immune system, which protects our body from various viruses and infections.
- Enabling Alpha to Beta Cell Conversion: As beta cells produce insulin, it is important to recover and rejuvenate beta cells for the complete reversal of type 1 diabetes, which can be done by converting alpha cells into beta cells. According to the data, there are 30% to 40% chances of reversal.
This approach will not only help in curing diabetes but also the major underlying cause of it: autoimmunity. Once this is treated, your body is fit and healthy and devoid of the risk of other autoimmunity diseases. The advantage of this treatment is that it focuses on mental health as well. As this type of diabetes is found in children, Dr. Gaurang Ramesh, while treating her patients, makes sure that the children are happy and the environment is also positive. A positive and happy mind helps in boosting the curing process, and the child recovers quickly. Most of the time, mental health is often neglected because of the unawareness of its effect on the body.
Conclusion
Although the underlying mechanisms for the development of multiple autoimmune diseases within the same person are unknown, recent progress suggests that common genetic factors or immunological processes are present among the different autoimmune diseases. Autoimmunity has provided clinically useful information; in particular, the indication of the presence of autoantibodies before the onset of clinical symptoms has made it possible to identify individuals at high risk of developing type 1 diabetes. Thus, to a very large extent, type 1 diabetes is a predictable disease.


.png)


