
People often get confused between IBS and IBD because both diseases almost have the same acronyms. Yet, they are both distinct digestive disorders. IBS stands for Irritable Bowel Syndrome, while IBD stands for Inflammatory Bowel Disease. IBD is a more serious cause for concern than IBS.
In specific cases, an individual may suffer from both IBS and IBD simultaneously, which is why; it is crucial to take a closer look at the symptoms and treatment of these two diseases.
In IBS, the lower part of the gastrointestinal (GI) tract (basically the small and large intestines, also called the small and large bowels) is affected. In IBD, there is inflammation in the tissues lining the digestive tract. Sores and ulcers are present in the lining of the large intestine and rectum.
Functional medicine can treat and manage IBD and IBS. Functional medicine takes into consideration the underlying causes of inflammation, optimizes the nutritional status of patients, and extends their remission periods (periods of good health after being ill).
So, What Causes IBS?
One or more of the following reasons may cause IBS:
- Changes in gut motility may cause IBS. Very strong or weak muscle contractions in the intestine can cause gas, bloating, diarrhea, etc.
- If the nerves in the digestive system don’t function properly due to various reasons.
- If there’s an overgrowth of bacteria in the intestine, meaning changes in gut microbiome
- People who have faced tremendous stress early in life are more susceptible to IBS.
- Certain foods may trigger symptoms of IBS.
- Repeated use of antibiotics might also lead to IBS. Sometimes the good bacteria are also killed along with the harmful bacteria.
_1728972222.webp)
What Causes IBD?
The exact causes behind IBD have not yet been ascertained. However, a few possible reasons are listed below:
- It could be the result of an immune system malfunction. As the immune system fights bacteria and viruses, the cells in the digestive tract can also become affected.
- Many IBD cases have hereditary patterns, though not all have a family history of the disease.
Factors that Aggravate IBD are as follows:
- Age: Most people develop symptoms of IBD while they are still under the age of 30.
- Medicines: Many non-steroidal anti-inflammatory medications may increase the chances of developing IBD.
- Stress: An increase in stress levels in patients was found to cause the disease to flare.
- Diet: Certain food items are found to be soothing the symptoms of IBD, while others worsen them.
Categorization of IBS and IBD
IBS is categorized into three types:
- IBS With Constipation (IBS-C): Stools are lumpy and hard.
- IBS With Diarrhea (IBS-D): Your faeces are loose and watery.
- IBS With Mixed Bowel Habits (IBS-M): On the same day, you may have both hard and lumpy stools and loose and watery stools.
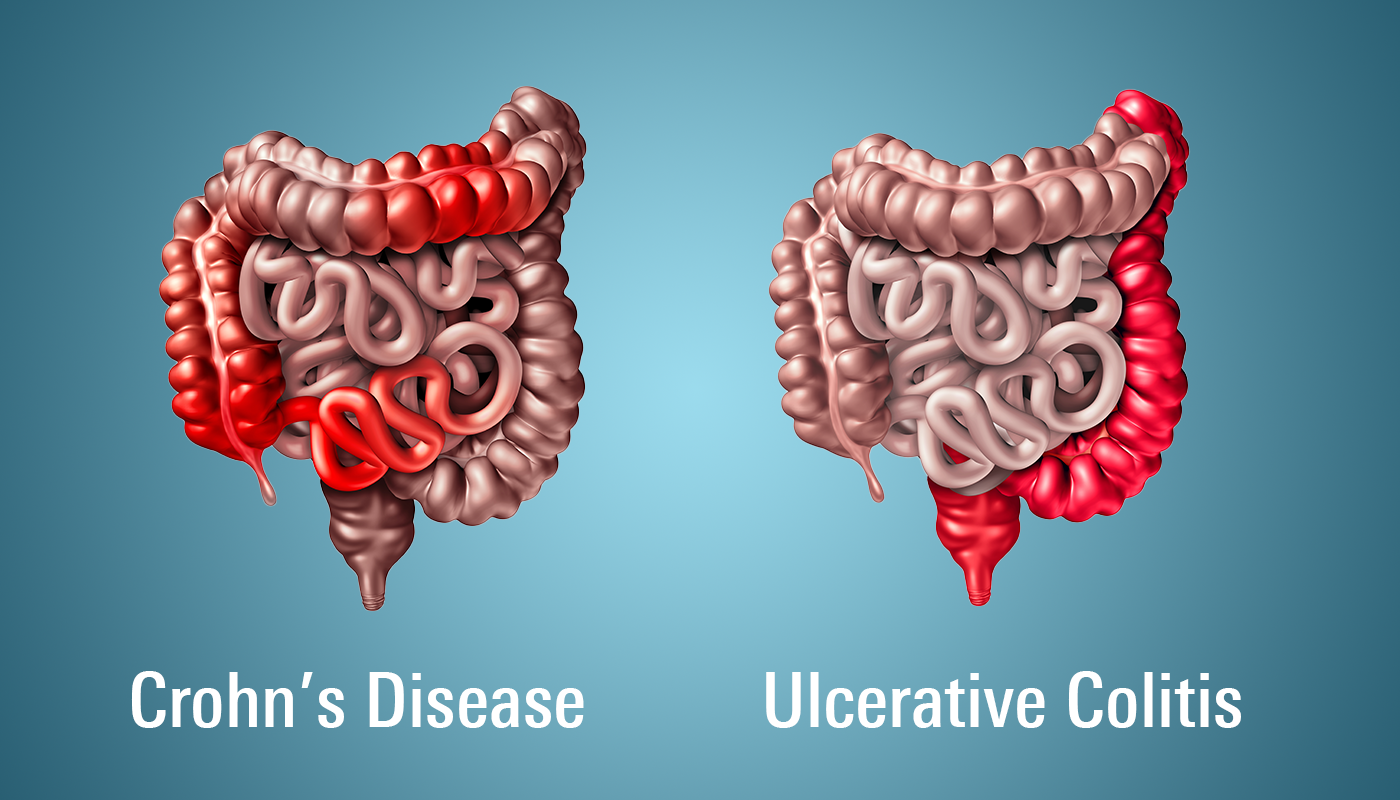
IBD is Categorized into Three Main Disorders:
- Crohn’s Disease: It is not yet clear what causes Crohn’s disease. In this disease, any portion of the gastrointestinal tract, including the mouth and the anus, can be impacted. All the layers of the digestive tract can be affected, and it often appears as several patches of inflamed tissue separated by healthy tissue. There is no known cure for Crohn’s disease. It can be managed at best.
Symptoms include anemia, pain or redness in the eyes, fatigue, fever, pain or soreness in the joints, nausea, loss of appetite, and red bumps under the skin. - Ulcerative Colitis: Small intestine and rectum linings are damaged by ulcerative colitis.
Symptoms include passing a small amount of blood in the stool, pain in the abdomen and cramps, pain in the rectum, and weight loss. There are also times when patients feel they need to urinate urgently but are unable to do so.
- Diverticulitis: This digestive system condition involves the inflammation or infection of one or more pouches in the intestine. It is also called colonic diverticulitis.
Symptoms include pain in the abdomen, bloating, blood in the stool, changes in bowel habits, constipation, diarrhea, nausea or vomiting, and a loss of appetite.
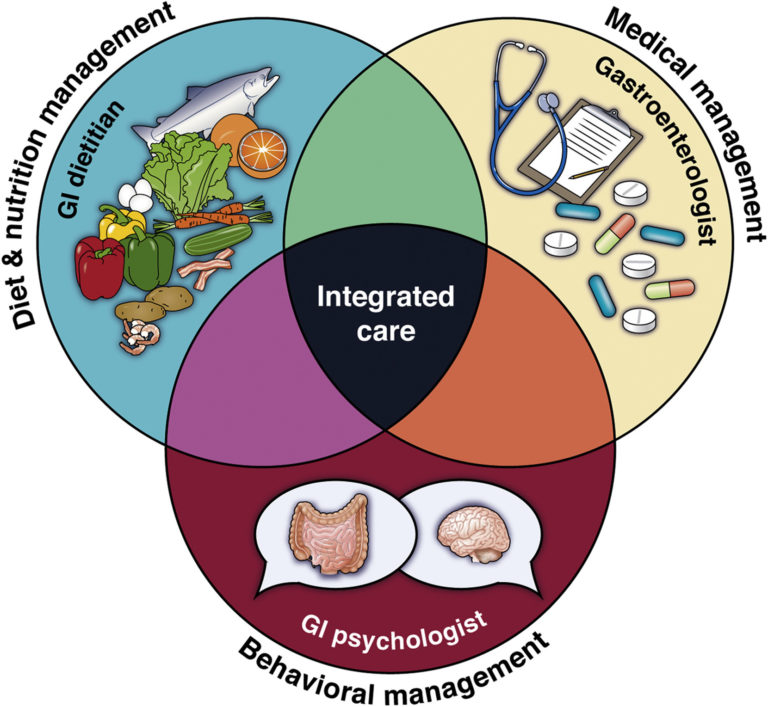
IBS and IBD Treatment Using Functional Medicine
From the perspective of functional medicine, a variety of treatments, including lifestyle changes, may enhance the quality of life for these individuals. Understanding the underlying causes of dysfunction and using treatments that address those causes is central to functional medicine.
Treatment for IBS
IBS is treated considerably differently by functional medicine than it is by traditional medicine. Functional medicine examines every area of digestion and nervous system health. It acknowledges that the cause of each person's IBS is different.
The following are the typical interventions that functional medicine practitioners recommend for IBS patients:
- Increasing Fibre Intake: Fibre-rich foods like broccoli, Brussels sprouts, chickpeas, split peas, etc., are introduced to the patient’s diet for quick healing.
- Not Using FODMAPS: The full form of FODMAPs is “fermentable oligosaccharides, disaccharides, monosaccharides, and polyols.” These are carbohydrates that are not very well or easily absorbed by the small intestine and thus can get stuck in the colon and give rise to infections. Foods high in these carbohydrates, like garlic, onions, baked beans, rye, wheat, etc., are not given to patients.
- Guided Elimination Diets: An elimination diet is designed to identify food allergies or sensitivities in patients so that their nutrition can be tailored accordingly. Additionally, it supports the gut microbiome. It is a 3-week-long program in which certain food items or categories of food are removed and then carefully reintroduced. This helps in creating a better and more efficient treatment module for the patient. The elimination diet, however, is not appropriate for everyone and should only be taken under the supervision of a functional medicine specialist.
- Maintaining hydration and increase in physical activity.
- Going for stress reduction methods.
- Using herbs and supplements based on lab results and the symptoms of each patient.

Treatment for IBD
Typical treatment protocol elements for IBD using functional medicine are as follows:
- Dietary studies are conducted to find any foods that might be causing or aggravating intestinal inflammation.
- Extensive analysis of gut microbiota (essentially microorganisms like bacteria, viruses, fungi, etc. in the gut) to search for any irregularities. A specialized diet and supplement regimen is developed to restore gut flora.
- Advice is given on therapeutic foods, herbs, and supplements that can help soothe inflammation.
- The nutritional state is fixed, and a tailor-made diet and supplement plan is designed to restore nutritional status.
Common Dietary Changes to be made for the Treatment of Both IBS and IBD
- Eat fibre-rich food
- Avoid dairy products
- Avoid food that makes you feel gassy or bloated
- Drink more water or consume foods that are rich in water, like cucumber, tomato, etc.
- Avoid caffeine

Conclusion
A functional medicine expert can help you create a health plan that is indeed evidence-based and specifically targeted to cure the symptoms of IBS or IBD in an individual. There are successful ways to control and manage IBS and IBD symptoms, whether you decide to utilize supplements, medications, nutrition, or lifestyle changes. Attend our workshop on digestive disorders to learn more.
Disclaimer: The information and other content provided in this blog, or in any linked materials, are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment. If you or any other person has a medical concern, you should consult with your healthcare provider.


.png)


