Your gut health and brain are more interconnected than you may think. The bidirectional relationship between the central nervous system and gut microbiota, also known as the gut-brain axis, has been of significant interest in recent years. Scientists believe that our gut microbiota can treat a number of disorders, such as Parkinson’s disease and depression. Here, we talk about the connection between gut health and brain health, how it works, and what happens when the balance is altered.
Gut Health and Brain – What’s the Relation?
The gut microbiome is sometimes referred to as the “second brain.” This is because a growing body of evidence suggests that our gut influences our health in ways that scientists are just now beginning to understand.
Research has established that the gut microbiota plays a critical role in different brain processes. It can also influence psychological processes such as mood and cognition.

Click to learn how protein affects our brain!
A healthy gut microbiota is essential for maintaining the healthy functioning of the microglia, a type of brain tissue. The microglia are responsible for maintaining brain health by removing unwanted cells, potential pathogens, and other waste materials. This helps reduce the risk of mental disorders like Parkinson’s disease, Alzheimer’s disease, prion diseases, multiple sclerosis, and HIV dementia.
But how does Gut Health influence Brain Function to such an extent?
The gut microbiome houses trillions of microbes in it. It may be hard to believe that the microbes in the gut collectively weigh as much as the adult human brain. Many of these microbes are important for brain development and function. They synthesize numerous neurotransmitters, such as GABA, serotonin, dopamine, and short-chain fatty acids. These compounds help regulate mood and appetite. The routes of communication between gut microbes and the brain are not fully understood yet, but they most likely include neural, endocrine, immune, and metabolic pathways.

Apart from these compounds, immune molecules such as cytokines are also produced in the gut. They can travel through the bloodstream and influence brain function in certain regions, such as the hypothalamus. Thus, the health of the gut microbiota may be a key triggering factor in the development of many brain disorders.
To summarize it in 3 points:
- Firstly, the gut and brain have many modes of communication.
- Secondly, microbes in the gut produce metabolites that can enter the blood, cross the blood-brain barrier, and have an influence on brain health.
- Lastly, gut microbes also have a big influence on the immune system.
Know how diet affects gut health here!
Gut Microbiome, Brain Health and the Development of Parkinson’s Disease
Parkinson’s disease is a progressive neurological condition that affects about 7–14 million people worldwide. In Parkinson’s, specific brain cells or neurons in the brain gradually die. Many of the symptoms are due to a loss of neurons that produce the neurotransmitter dopamine. Low dopamine levels cause abnormal brain activity, leading to the development of Parkinson’s.

Many Parkinson’s patients notice changes in their digestion. Research suggests that changes in the gut may be more than just a symptom. There is mounting evidence that some of the earliest symptoms of PD may actually start in the gut.
The formation of a clump of proteins (alpha-synuclein) in the brain plays a major role in the progression of Parkinson’s. Dopamine-producing neurons within the substantia nigra are susceptible and vulnerable to the accumulation of alpha-synuclein. The protein may also play a role in the progression of autonomic disorders of the cardiovascular and gastrointestinal systems that have an association with Parkinson’s.
Supporting Studies
In a study published in Cell (2016), researchers studied the effects of removing bacteria from the gut and their impact on disease susceptibility. In the study, mice with increased alpha-synuclein were raised in a germ-free environment. This prevented the normal development of the gut microbiota. Researchers found that these mice developed the symptoms of Parkinson’s much later than normal. This proves that the health of the gut microbiome can affect the progression of Parkinson’s.
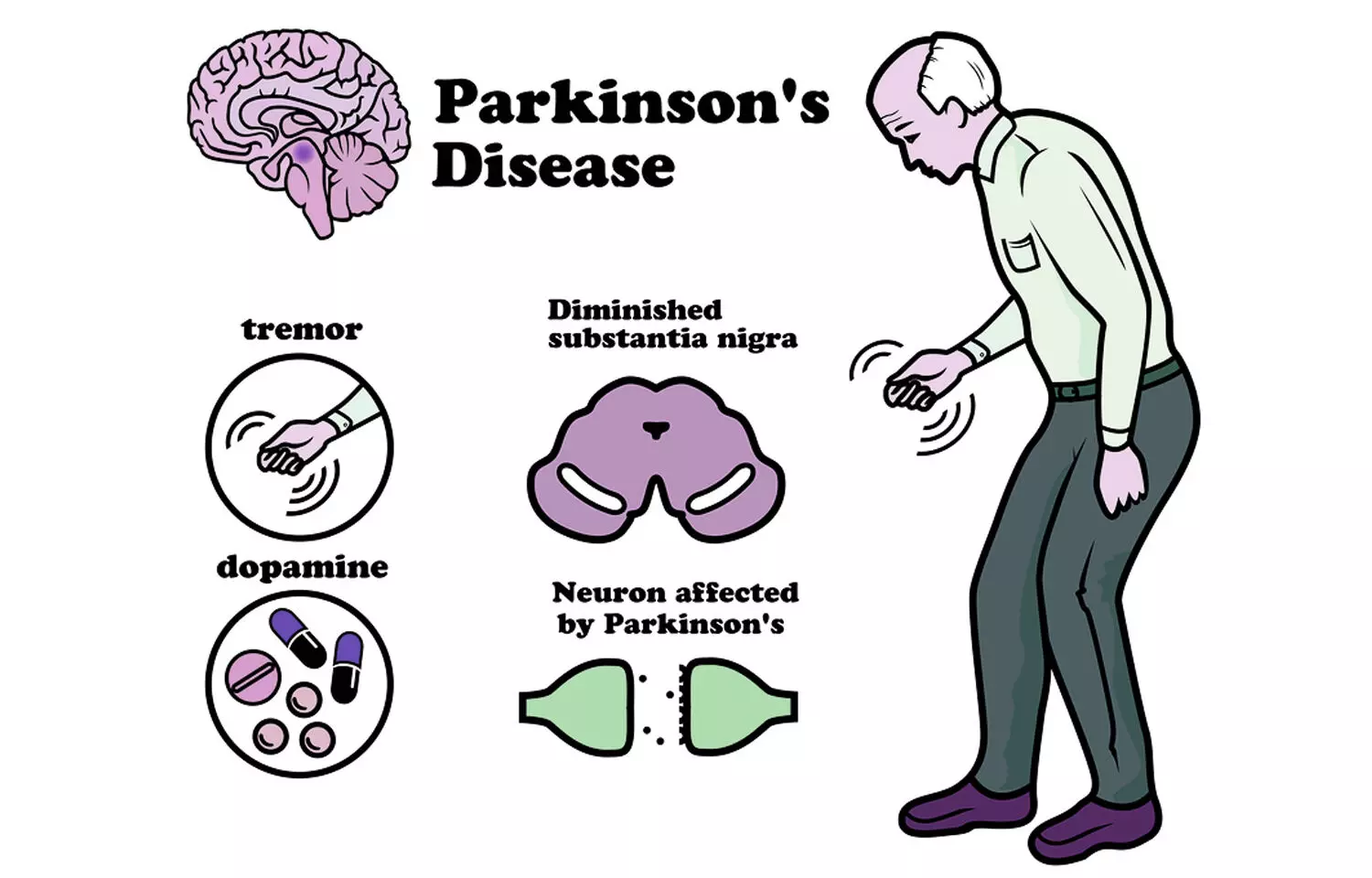
This research provides key insights into the causes of Parkinson’s. It also forces us to look from a different point of view. Moreover, it shows how lifestyle and environmental factors affect your gut microbiota, influencing the risk of Parkinson’s.
Evidence of the involvement of the gut in Parkinson’s comes from a procedure for the treatment of peptic ulcers. It involves cutting the information flow between the gut and the brain by cutting the vagus nerve, which connects the brain to the body. The risk of developing Parkinson's was reduced in individuals who underwent the procedure. This stopped the flow of alpha-synuclein clumps from the gut to the brain. These findings and studies have urged researchers to rethink where Parkinson’s actually originates.
Gut Vitality in Autism Spectrum Disorder (ASD)
Autism Spectrum Disorder (ASD) is a group of neurodevelopmental disorders that include problems with communication and social interaction. People with autism often demonstrate restricted and repetitive patterns of behavior.
Gastrointestinal symptoms are a common problem in patients with ASD. Many studies have shown alterations in the composition of the fecal microbes and metabolic products of the gut microbiome in autism patients. Autism patients had a higher percentage of abnormal intestinal permeability.
Studies suggest that autistic people have twice the amount of yeast in their bodies as compared to healthy individuals. The yeast present in the gut, such as Candida albicans, absorbs fewer carbohydrates and minerals. However, it releases higher amounts of toxins and ammonia, which can induce autistic behavior. Studies also suggest that the interaction of propionic acid and ammonia released by this yeast can produce an excessive amount of beta-alanine, an important contributor to autism.
A fundamental factor underlying the relationship between autism and the gut is the increased permeability of the intestinal tract of ASD individuals, also known as a “leaky gut." Several studies propose that autistic animals experience defects in the gastrointestinal barrier. This results in the entry of toxins and bacterial products into the bloodstream, which influences brain function. For example, lipopolysaccharide (LPS) components of certain bacteria increase in the blood of autistic individuals compared to healthy individuals. LPS components contribute to impaired social-behavioral scores in autism patients.
Stress Affects Gut Health and Brain Function
Stress influences both gut health and brain function. Several studies provide new insights into how the microbiota is responsible for regulating brain development and function.
Results of animal studies have shown that stress and emotions cause the brain to influence the microbial composition of the gut. This is due to the release of neurotransmitters that influence the physiology of the gut and alter the microbiota habitat. Stress hormones such as noradrenaline released in the gut may influence bacterial gene expression or signaling between bacteria.
:max_bytes(150000):strip_icc()/synapse-103018523-59c7f273054ad9001175c403.jpg)
Additionally, neurotransmitters such as serotonin, Gamma-Aminobutyric Acid (GABA), and dopamine secreted by gut bacteria play a key role in regulating mood. Several studies using germ-free mice show that animals having no microbiota have impaired social behavior as well as anxiety and stress. Furthermore, it has been observed that certain behaviors brought on by the absence of gut microbiota correlate with neurochemical changes in the brain.

Data obtained using germ-free animals have shown that neurogenesis is also regulated by the microbiome. Furthermore, the gut microbiota affects both structural and functional changes in the amygdala.
Although the results are from animal studies and few observational human studies, there is enough evidence to prove that the development and functioning of the brain are dependent on the diversity and structure of the gut microbiota.
Conclusion
Thus, it is clearly evident that our gut and brain function are closely related. Our gut microbiome regulates several critical brain functions. Maintaining a healthy gut by eating a healthy diet and reducing stress levels can help reduce the risk of mental health issues like Parkinson’s and ASD.


.png)


