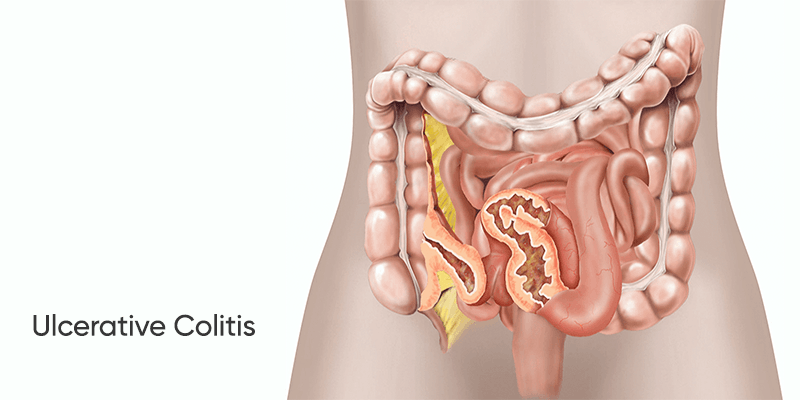
Ulcerative colitis is a chronic inflammatory condition affecting the large intestine and rectum. It occurs when the immune system mistakenly attacks healthy cells, leading to inflammation, ulcers, and a range of uncomfortable symptoms. While it can affect people at any age, it is most common in young adults. For some, traditional medical treatments may not provide adequate relief. Functional medicine offers a promising approach to managing ulcerative colitis, focusing on improving overall well-being and reducing symptoms. It's important to note that ulcerative colitis and Crohn's disease are both types of inflammatory bowel diseases (IBD), but they have distinct characteristics.
The study by AIG Hospitals in Hyderabad showed that about 15 lakh people in India suffer from IBD, but the true picture is not clear due to a lack of proper data.
Causes and Risk Factors for Ulcerative Colitis
Ulcerative colitis is a chronic inflammatory condition caused by an overactive immune system mistakenly attacking the tissues of the large intestine and rectum. While the exact cause is complex, several factors can increase your risk:
- Age: Most people are diagnosed between 15 and 30 years old or after 60.
- Race and Ethnicity: Individuals of white ethnicity, especially those of Ashkenazi Jewish descent, have a higher risk.
- Genetics: A family history of ulcerative colitis or Crohn's disease increases your susceptibility.
- Gut Microbiome: Differences in the gut microbiome, the ecosystem of bacteria, viruses, and fungi in the digestive system, have been linked to ulcerative colitis.
While stress and diet may not directly cause ulcerative colitis, they can trigger symptom flares. Identifying and avoiding these triggers can help manage the condition effectively.
Functional Medicine Approach to Ulcerative Colitis
Functional medicine recognizes that the body is an interconnected system and seeks to identify underlying imbalances that may contribute to ulcerative colitis symptoms. By addressing these imbalances, functional medicine can help:
- Reduce Inflammation: Functional medicine interventions can help reduce inflammation in the digestive tract, alleviating symptoms like abdominal pain, diarrhea, and bleeding.
- Support Gut Health: By optimizing gut function and promoting a healthy gut microbiome, functional medicine can help restore balance and reduce inflammation.
- Improve Overall Health: Functional medicine addresses nutritional deficiencies, supports immune function, and promotes stress management, all of which can contribute to improved overall health and well-being.
A functional medicine approach to ulcerative colitis may involve:
- Dietary Modifications: Identifying and eliminating trigger foods, while incorporating foods that support gut health and reduce inflammation.
- Nutritional Supplements: Addressing nutritional deficiencies and supporting digestive function with targeted supplements.
- Lifestyle Changes: Managing stress, improving sleep, and engaging in regular physical activity can help optimize overall health.
- Gut Microbiome Support: Strategies to promote a healthy gut microbiome, such as probiotics and prebiotics.
- Addressing Underlying Conditions: Identifying and addressing any underlying health conditions that may contribute to ulcerative colitis symptoms.
By taking a holistic approach, functional medicine can help individuals with ulcerative colitis experience improved symptoms, better quality of life, and potentially even remission.
Take Away
Ulcerative colitis is a chronic inflammatory condition affecting the large intestine and rectum. While conventional treatments can provide relief, functional medicine offers a comprehensive approach that addresses the underlying causes of the condition. By optimizing gut health, reducing inflammation, and supporting overall well-being, functional medicine can help individuals with ulcerative colitis experience improved symptoms and a better quality of life.
Disclaimer: The information and other content provided in this blog, or in any linked materials, are not intended and should not be construed as medical advice, nor is the information a substitute for professional medical expertise or treatment. If you or any other person has a medical concern, you should consult with your healthcare provider.
