There are two types of diabetes: type 1 and type 2 diabetes. India’s rapid economic growth and modernization have led to drastic lifestyle changes for all of us. It has prompted us to lead a sedentary lifestyle and indulge in more western junk foods such as burgers and pizzas. These changes have increased obesity and its related health problems, such as diabetes. Several young children and teenagers are victims of diabetes these days, as are middle-aged people. But there is a difference!
Here we list out some of the basic differences between type 1 and type 2 diabetes and what you can do to manage them.
Most children and adolescents suffer from type 1 diabetes, while most adults suffer from type 2 diabetes.
What are Type 1 and Type 2 Diabetes?
Type 1 diabetes is also known as juvenile-onset diabetes because it often begins in childhood. It is an auto-immune disorder that attacks the insulin-producing cells (beta cells) present in the pancreas, affecting the production of insulin hormones. This increases the blood glucose (blood sugar) level in the body, causing diabetes. Type 1 diabetes generally occurs due to genetic predisposition.
Type 2 diabetes accounts for 95% of diabetes in adults. It is known as adult-onset diabetes, but due to increasing obesity and overweight issues, many teenagers are also suffering from it. In type 2 diabetes, the pancreas produces insulin, but the amount produced is not sufficient for the body due to insulin resistance or a lack of insulin sensitivity. When the body produces insulin under conditions of insulin resistance, the cells fail to respond normally to the insulin hormone. Insulin resistance can be caused by genetic and lifestyle factors.

What causes Type 1 and Type 2 Diabetes?
If a family member of yours suffers from type 1 diabetes, then you’re at higher risk of developing it. This is because genetic factors are primarily the reason behind type 1 diabetes. It could also be the result of faulty beta cells in the pancreas that normally produce insulin.
The cause of type 2 diabetes is genetic or lifestyle factors, or sometimes both. The most common contributing factors to type 2 diabetes are:
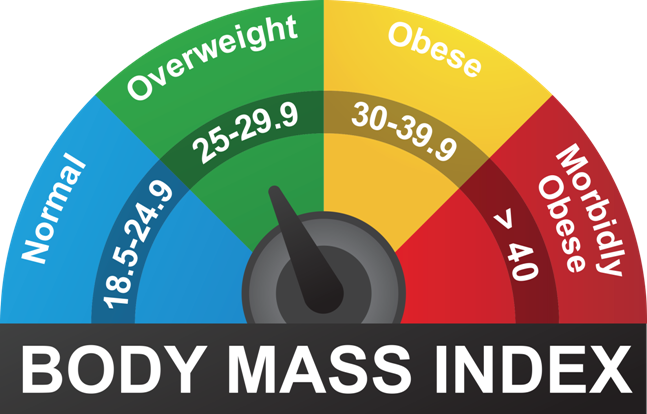
- Obesity: People who are obese or overweight are at a higher risk of developing type 2 diabetes. If the BMI (Body Mass Index) of a person is between 25 and 29.9, they are overweight. If the BMI is 30 or more, they are obese.
- High blood pressure: Individuals suffering from high blood pressure or high blood cholesterol levels are at a higher risk of type 2 diabetes. About 80% of people with type 2 diabetes have high blood pressure.
- High blood cholesterol: Researchers have found that high blood cholesterol levels are linked to type 2 diabetes and vice versa.
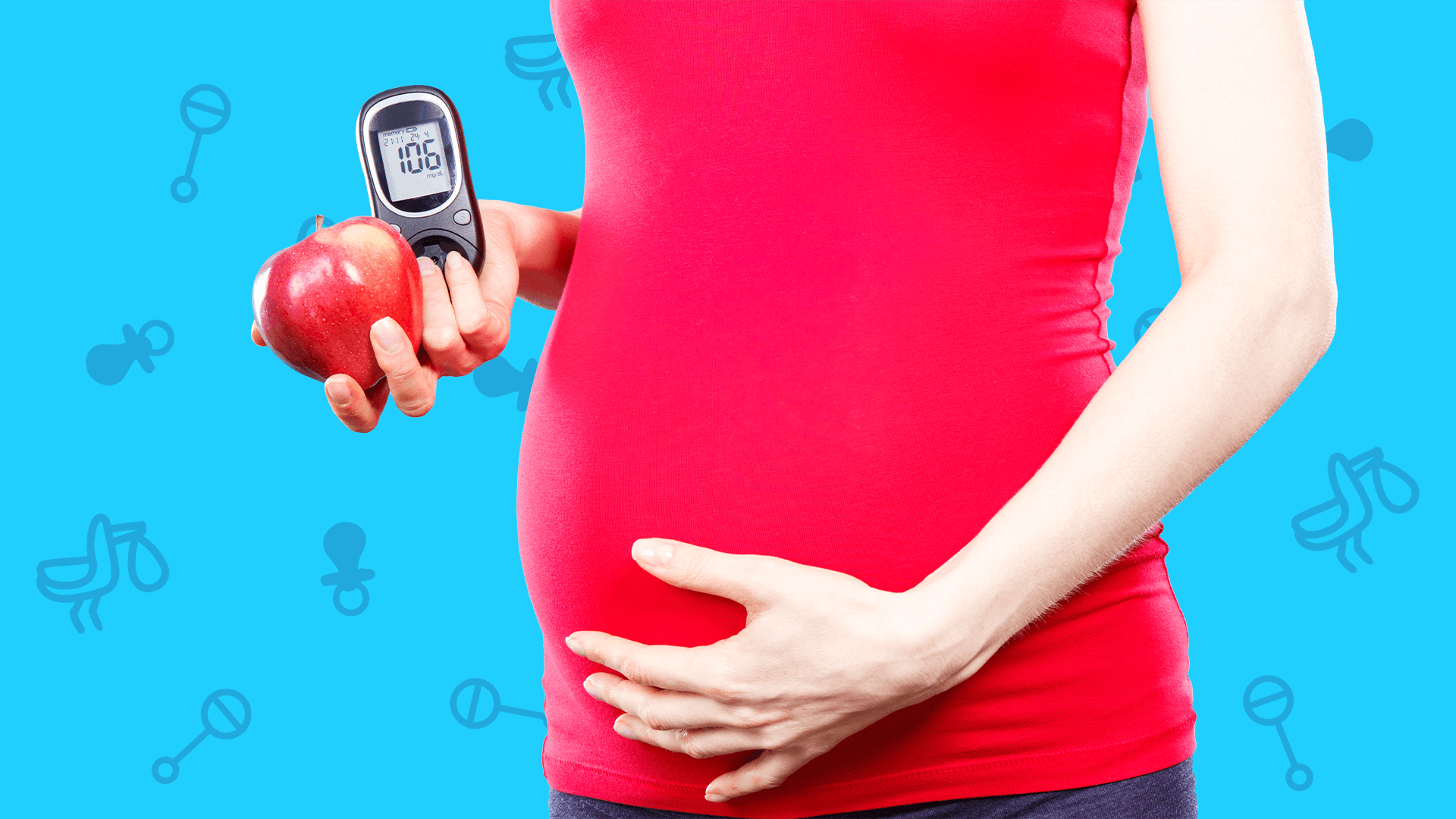
- Gestational diabetes: Gestational diabetes refers to elevated blood sugar during pregnancy for women who have not had diabetes prior to pregnancy. 5-10 % of mothers who had gestational diabetes will have type 2 diabetes after pregnancy. However, if not, there is a 20- 50% chance of developing type 2 diabetes within the next 10 years.
- Ageing: The risk and prevalence of type 2 diabetes increase with age. This can be due to decreased beta cell activity, or beta cell proliferation (an increase in beta cells from beta cell replication), or decreased insulin sensitivity in the body.
- Lack of physical activity: Daily physical activity like exercising helps control body weight and composition, reducing the risk of type 2 diabetes.
How can you manage Type 1 and Type 2 Diabetes?
Type 1 diabetes is a serious health condition, and you can manage it in the following ways:
- Insulin replacement can be achieved through lifelong insulin injections (up to 6 every day) or the use of an insulin pump.
- Monitoring of blood glucose levels regularly (up to 6 times every day or as directed by your doctor).
- Following a healthy diet and eating plan.
- Regular physical activity or exercise.
You can manage type 2 diabetes initially through lifestyle modification, including a healthy diet, regular exercise, and monitoring your blood glucose levels. It is because:
- Eating well helps manage your blood glucose levels and your body weight.
- Exercising helps the insulin to work more effectively, lowers your blood pressure, and reduces the risk of heart disease.
- Blood glucose tests at regular intervals help in monitoring the effectiveness of your diabetes treatment.
However, sometimes healthy eating and exercise are not enough to keep the blood glucose levels down. As time progresses, in type 2 diabetes, the insulin becomes more resistant and the pancreas is less effective at converting glucose into energy. To help the pancreas convert glucose into energy, people with type 2 diabetes are often prescribed tablets.
Read more about managing diabetes with diet and exercise here!
Conclusion
Thus, with proper diet, exercise, and periodic blood glucose monitoring, both type 1 and type 2 diabetes can be controlled. The aim of diabetes management is to keep blood glucose levels as close to the optimum range as possible. However, the ranges will vary depending on the individual and their needs.
Disclaimer: Consult a health expert to help you with blood glucose monitoring, healthy eating, and physical activity. Occasionally, side-effects can occur with medication. Insulin injections and other medications are compulsory in some cases, and diet cannot be a substitute.


.png)


